Abstract
Hypomethylating agents (HMA), namely azacitidine and decitabine, are used for treatment of MDS and AML. Although HMAs have demonstrated efficacy in a subset of patients, their mechanism of action is not well established. Some studies indicate that HMAs induce expression of specific target proteins, thus enhancing the efficacy of targeted therapies. For example, studies of HMAs used in combination with gemtuzumab ozogamicin (GO) suggest that they can apply additional epigenetic stress to AML cells and increase surface CD33 expression, thereby increasing the efficacy of GO. Despite suggestions of epigenetic modulation of target antigens, data on comprehensive response to HMAs is lacking. We proposed to evaluate the full extent of surface antigen expression in different AML cell lines after prolonged exposure to azacitidine.
The dose and duration of azacitidine therapy used for prolonged exposure was established in Kasumi-1 cells (t(8;21), N822K KIT mutation). A daily dose of 250 nM allowed continued cellular proliferation for 18 days. We then treated two cell lines, Kasumi-1 and MV4-11 (t(4;11), FLT3 -ITD+) as above for 14-18 days. Cells were submitted for multi-dimensional flow cytometry (MDF) every 2-4 days.
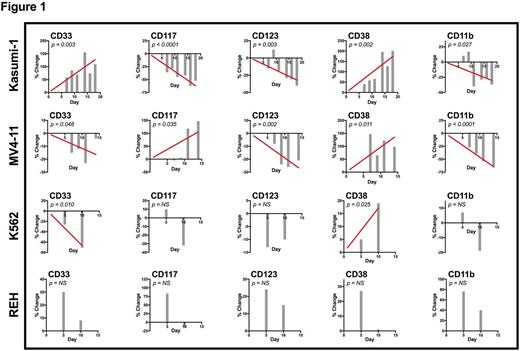
Prolonged azacitidine exposure resulted in broad changes in hematopoietic cell surface antigens, as demonstrated by MDF analysis. CD33, the premier cell surface target for AML immunotherapy, increased significantly in Kasumi-1 cells, approximately doubling by day 14 of treatment (p=0.003, Fig. 1). C -kit, or CD117, which is overexpressed in Kasumi-1 cells and is a potential target of tyrosine-kinase inhibitor (TKI) therapy in t(8;21) AML, was significantly decreased with azacitidine exposure (p <0.0001, Fig. 1). In contrast, treatment of MV4-11 cells resulted in significant decrease in CD33 with a corresponding increase in CD117 (Fig. 1).
Kasumi-1 and MV4-11 both exhibited significant increases in surface CD38, CD13, and CD36, and significant decreases in CD64, CD123, and CD11b. Cell marker changes observed in only one cell line include significantly increased CD34 in Kasumi-1 and significantly increased CD56 in MV4-11. Many of the observed changes peaked after day 10 of treatment. No significant changes were seen in either line in CD7, CD14, CD16, CD19, CD45, and HLA-DR. Notably, the shared pattern of surface antigen changes in both Kasumi-1 and MV4-11 indicates that prolonged azacitidine exposure may induce a less mature myeloid phenotype, as typified by increased CD38 and decreased CD11b and CD123 (Fig. 1).
The results above were validated in an experiment in which 4 leukemia cell lines were exposed to azacitidine as above for 10 days, with MDF analyses on days 5 and 10. Cell lines included Kasumi-1, MV4-11, K562 (t(9;22)), and the ALL cell line REH (t(12;21)). Similar trends in surface antigens for Kasumi-1 and MV4-11 were again observed. K562 cells exhibited increased CD38, CD36, CD7, CD14, and CD19, and decreased CD33, CD56, CD64, and CD45 (Fig. 1). No change was seen in K562 in CD117, CD13, CD11b, CD16, CD34, CD123, and HLA-DR (Fig. 1). Of these myeloid markers tested, REH cells had only a significant increase in CD13, a marker also seen in very early B-lymphocytes. Thus, HMAs do not appear to promote lymphoid to myeloid phenotype shift in REH.
We observed broad changes in cell surface antigen expression in myeloid leukemia cell lines treated with prolonged azacitidine, which may signify changes in gene expression induced by hypomethylation. Among AML cell lines, prolonged azacitidine exposure resulted in a less mature immunophenotype. We observed significant changes in CD33 and CD117, both of which are considered potential therapeutic targets in AML. CD33 expression was increased by azacitidine exposure in Kasumi-1 cells, and reduced in MV4-11 and K562. C -kit was also noted to variably change in response to azacitidine. Downregulation of cell surface antigens is a known resistance mechanism to immunotherapeutic agents, including antibody-drug conjugates such as GO. Resistance to c -kit-targeted agents has been proposed to occur through a variety of mechanisms, including cell surface expression, therefore changes to c -kit levels induced by HMAs may be an important avenue of investigation in averting TKI resistance. The use of prolonged, low-dose hypomethylating agents warrants further investigation as a potential means to modulate surface protein levels for therapeutic benefit.
Pardo: Hematologics Inc: Employment. Loken: Hematologics Inc: Employment, Equity Ownership. Brodersen: Hematologics Inc: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal